“Advancing Lung Health in North Carolina”
North Carolina Thoracic Society Newsletter
Summer 2022
NCTS Events and Announcements
“Digital Health in Respiratory Diseases” on Saturday Sept 24 on the Duke University campus, under the direction of Mashael Al-Hegelan, MD and Praveen Mannam, MD. Topics on the agenda include remote digital monitoring for OSA, digital inhalers, cybersecurity, virtual pulmonary rehabilitation, remote digital oscillometry, and “wearables” for lung diseases.
Our keynote is Richard Costello, MD (Royal College of Surgeons Ireland) who will present on his journey to develop, investigate and apply digital health in respiratory practice.
Registration: https://www.eventbrite.com/e/digital-health-in-respiratory-diseases-tickets-374468694947
NCTS will facilitate teleconferences entitled: “Management Strategies for Mycobacterium Avium Complex Infections: Diagnosis and Treatment of a Growing Health Threat”. Details will be announced via email.
Lung Health in North Carolina Vaping
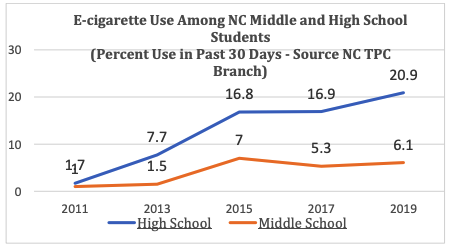
The figure shows vaping rates in young persons are growing in NC (Figure), yet sales are illegal in North Carolina in those < 21 yo. Fruity and most other flavors have been removed, while nicotine, menthol, and other additives persist.
Today, safety is largely based on the long term effects of current ingredients discussed below and if a new wave of illicit toxins in e-cigarettes comes along. Several recent papers have been published on acute and long-term effects of vaping, including reporting small airways fibrosis. The 2018 EVALI epidemic led some to believe that cigarettes are safer.
There is no consensus on e-cigarettes for smoking cessation. While some studies show them effective for smoking cessation, others do not. Clearly, persons starting with e-cigarettes can end up addicted to smoking tobacco. A recent study in JAMA polling 2300 physicians including 175 pulmonologists on e-cigarette and vaping issues. E-cigarettes were recommended for smoking cessation by 17% of pulmonologists, predominantly in recalcitrant current smokers. National Health Service in England is now considering permitting e-cigarettes for smoking cessation (Chest Physician July 2022). The debate goes on.
- E-Cigarette Use, Small Airway Fibrosis, and Constrictive Bronchiolitis Hariri, Lida P.; Flashner, Bess M.; Kanarek, David J. et al…
NEJM evidence, 05/2022, Volume 1, Issue 6 - Delnevo, C. D., Jeong, M., Teotia, A., Bover Manderski, M. M., Singh, B., Hrywna, M., Wackowski, O. A., & Steinberg, M. B. (2022). Communication Between US Physicians and Patients
Regarding Electronic Cigarette Use. JAMA network open, 5(4), e226692. https://doi.org/10.1001/jamanetworkopen.2022.6692
Dr Lisa Norman, a Novant Health pathologist and advocate for public education on e-cigarettes and Dr Joe Mammarappallil, MD a cardiothoracic radiologist with Duke University, provide their perspectives below. We also share some great resources from Stanford University to educate the public, including the young.
Vaping-related Educational Materials
Stanford University vaping toolkit — education of adolescents, teenagers, and adults. The link and some of the powerpoints (with speaker notes) are below.
E-Cigs/Vapes & Pod-Based | Tobacco Prevention Toolkit | Stanford Medicine
Vaping-Induced Lung Injuries
Lisa Norman, MD (Pathologist – Novant Health and advocate for educating
the public on e-cigarettes)
Lisa Norman, MD (Pathologist – Novant Health and advocate for educating the public on e-cigarettes) Vaping associated pulmonary injury (VAPI), also called e-cigarette or vaping product use associated lung injury (EVALI) emerged as a public health issue in 2018. EVALI is an acute or subacute respiratory illness that is characterized by a spectrum of acute lung injury patterns that range from organizing pneumonia to acute fibrinous pneumonitis to diffuse alveolar damage. Vitamin E acetate in bootleg THC for vaping was thought to be the primary source of EVALI.
spitalized patients. While these lung injury patterns are non-specific and other etiologies must be excluded, the clinical history of vaping is critical information in forming a differential diagnosis to determine the root cause. Additionally, a condition referred to as “popcorn lung” (bronchiolitis obliterans) has also been associated with vaping. This disease damages and scars lung tissue permanently and is irreversible once it constricts the airways. Aside from various forms of acute lung injury, seizures, loss of taste (“vape tongue”), and increased risk of strokes, heart disease, and death have been reported.
E-cigarettes use e-liquid that generally contains predominantly propylene glycol and glycerin in conjunction with nicotine, flavorings, additives, and differing amounts of contaminants. Some also contain cannabidiol or cannabis oil but the precise composition is rarely known. Studies have shown that e-liquid also contains formaldehyde and the average vaper is exposed to one microgram per day. Formaldehyde is a strong smelling colorless gas which is a highly toxic systemic poison absorbed by inhalation. When dissolved in water it is called formalin which serves as an industrial disinfectant and a preservative in funeral homes and medical labs. Pathology specimens are routinely preserved in a formalin fixative. A study led by Harvard School of Public Health found two chemicals widely used to flavor e-liquid are diacetyl and 2,3 pentanedione. Diacetyl may impair cilia in the human airway, which function as a first line of defense in the lungs and has been linked to “popcorn lung.” It is shocking that these sorts of toxic chemicals are components of e-liquids and proves the lack of federal regulation in this industry. There has been a marketing blitz within the vaping industry specifically targeting our youth, designed to steal their health. Autopsy studies have shown that as today’s young vapers grow older and develop comorbidities, there is also serious risk for chronic lung damage. However, further research is necessary to continue to collect data in the evaluation of both acute and chronic vaping effects on the body, at both the gross and microscopic examination level. Scientific studies are slow to keep up with the rapid pace of the rising vaping epidemic and there remains much work to be done. However, at this point evidence supports that vaping can be a serious health hazard. Proper education of our youth is paramount to help them fully understand the potential devastating consequences of this dangerous habit.
Descriptions of the pathology underlying the conditions is limited to findings in surgical specimens of hospitalized patients. While these lung injury patterns are non-specific and other etiologies must be excluded, the clinical history of vaping is critical information in forming a differential diagnosis to determine the root cause. Additionally, a condition referred to as “popcorn lung” (bronchiolitis obliterans) has also been associated with vaping. This disease damages and scars lung tissue permanently and is irreversible once it constricts the airways. Aside from various forms of acute lung injury, seizures, loss of taste (“vape tongue”), and increased risk of strokes, heart disease, and death have been reported.
E-cigarettes use e-liquid that generally contains predominantly propylene glycol and glycerin in
conjunction with nicotine, flavorings, additives, and differing amounts of contaminants. Some also contain cannabidiol or cannabis oil but the precise composition is rarely known. Studies have shown that e-liquid also contains formaldehyde and the average vaper is exposed to one microgram per day. Formaldehyde is a strong smelling colorless gas which is a highly toxic systemic poison absorbed by inhalation. When dissolved in water it is called formalin which serves as an industrial disinfectant and a preservative in funeral homes and medical labs. Pathology specimens are routinely preserved in a formalin fixative.
A study led by Harvard School of Public Health found two chemicals widely used to flavor e-liquid are diacetyl and 2,3 pentanedione. Diacetyl may impair cilia in the human airway, which function as a first line of defense in the lungs and has been linked to “popcorn lung.” It is shocking that these sorts of toxic chemicals are components of e-liquids and proves the lack of federal regulation in this industry. There has been a marketing blitz within the vaping industry specifically targeting our youth, designed to steal their health.
Autopsy studies have shown that as today’s young vapers grow older and develop comorbidities, there is also serious risk for chronic lung damage. However, further research is necessary to continue to collect data in the evaluation of both acute and chronic vaping effects on the body, at both the gross and microscopic examination level. Scientific studies are slow to keep up with the rapid pace of the rising vaping epidemic and there remains much work to be done. However, at this point evidence supports that vaping can be a serious health hazard.
Proper education of our youth is paramount to help them fully understand the potential devastating consequences of this dangerous habit.
- Cecchini MJ, Boland JM, Larsen BT et al. “Interstitial lung diseases associated with smoking. Vaping associated acute lung injury.” PathologyOutlines.com, Inc. 04-12-22.
https://www.pathologyoutlines.com/topic/lungnontumorvaping.html - Mukhopadhyay S, Mehrad M, Dammert P et al. “Lung biopsy findings in severe pulmonary illness associated with e-cigarette use (vaping).” Am J Clin Pathol. 2020 Jan 1;153(1):30-39.
DOI:10.1093/ajcp/aqz182. https://pubmed.ncbi.nlm.nih.gov/31621873 - Zulfiqar H and Rahman O. “Vaping associated pulmonary injury.” NCBI Bookshelf. StatPearls1. Publishing, 01-07-22. https://www.ncbi.nlm.nih.gov/books/NBK560656/
- Marsden L, Michalicek Z, and Christensen E. “More on the pathology of vaping-associated lung injury.” N Engl J Med 2020; 382:387-390. DOI: 10.1056/NEJMc1914980
- Priemer D, Gravenmier C, Batouli A, and Hooper JE. “Overview of pathologic findings of vapingin the context of an autopsy patient with chronic injury.” Arch Pathol Lab Med 2020 Nov 1;144(11):1408-1413. DOI: 10.5858/arpa.2019-0637-RA.
https://pubmed.ncbi.nlm.nih.gov/32383974
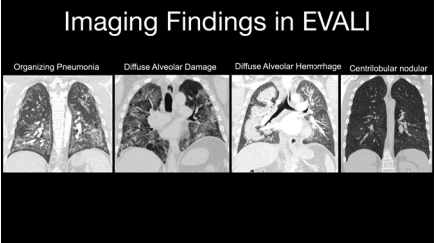
THE IMAGING FINDINGS OF VAPING ASSOCIATED LUNG DISEASE
Joe Mammarappallil, MD, PhD (Assistant Professor of Radiology/Cardiothoracic Imaging, Duke University School of Medicine) Vaping-associated lung disease, or EVALI (e-cigarette or vaping product use-associated lung injury) The exact incidence of EVALI is unclear with most symptomatic cases involving the combined usage of nicotine with cannabinoid products. Patient symptomatology mirrors other inhalation lung injury presentations including shortness of breath, chest pain, cough with or without fever.
As with many chronic lung diseases, the imaging patterns of EVALI appear variable. In a highly cited article about the imaging patterns of EVALI, TS Henry et al. describe four imaging patterns seen in patients who met criteria for having vaping-associated lung injury. The imaging patterns identified in this study were: 1. Acute Eosinophilic Pneumonia. 2. Diffuse Alveolar Damage. 3. Organizing Pneumonia 4. Lipoid Pneumonia. In some cases, imaging patterns were found to overlap in the same patient. It is helpful to organize these imaging patterns into acute and more chronic appearing lung injuries. Acute/rapid lung injury can often have the imaging appearance of acute eosinophilic pneumonia and diffuse alveolar damage that are often associated with inhalation injuries. The imaging appearance of acute eosinophilic pneumonia is often characterized by ground glass opacities and consolidation often associated with interlobular septal thickening and pleural effusions. Imaging findings of diffuse alveolar damage demonstrate centrilobular ground glass opacities/nodules with or without consolidation often with subpleural sparing. In subacute EVALI, findings of lipoid pneumonia can be visualized often 4 demonstrating a basilar process of ground glass opacities with irregular consolidation and “crazy paving”. Chronic EVALI can have imaging findings of organizing pneumonia which will often show a peripheral process of ground glass/consolidation sometimes demonstrating the reverse halo/atoll sign. Although the imaging findings of EVALI can be variable, correlating specific imaging findings described finding with patient histories will likely triage these patients appropriately.
REFERENCES:
- Centers for Disease Control and Prevention. Outbreak of Lung Disease Associated with E-Cigarette Use, or Vaping. Accessed 3 June 2020.
- Christiani DC. Vaping-Induced Lung Injury. (2019) The New England journal of medicine. doi:10.1056/NEJMe1912032 – Pubmed
- Layden JE, Ghinai I, Pray I, Kimball A, Layer M, Tenforde M, Navon L, Hoots B, Salvatore PP, Elderbrook M, Haupt T, Kanne J, Patel MT, Saathoff-Huber L, King BA, Schier JG, Mikosz CA, Meiman J. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin – Preliminary Report. (2019) The New England journal of medicine. doi:10.1056/NEJMoa1911614 – Pubmed
- Maddock SD, Cirulis MM, Callahan SJ, Keenan LM, Pirozzi CS, Raman SM, Aberegg SK. Pulmonary Lipid-Laden Macrophages and Vaping. (2019) The New England journal of medicine. doi:10.1056/NEJMc1912038 – Pubmed
- Henry TS, Kanne JP, Kligerman SJ. Imaging of Vaping-Associated Lung Disease. (2019) The New England journal of medicine. doi:10.1056/NEJMc1911995 – Pubmed
- Agustin M, Yamamoto M, Cabrera F, Eusebio R. Diffuse Alveolar Hemorrhage Induced by Vaping. (2018) Case reports in pulmonology. 2018: doi:10.1155/2018/9724530 – Pubmed
CLINICAL PRACTICE
Inhalers and Drug Interactions with Paxlovid®
Prepared by Roy Pleasants, PharmD
The purpose of this brief report is to discuss drug interactions between Paxlovid® (nirmatrelvir/ritonavir) and inhaled medicines. Ritonavir is used as a “booster” by inhibiting Cytochrome P450 3A4 metabolism of nirmatrelvir, increasing its blood levels. For inhaled medicines, pertinent sites of CYP3A4 metabolism are in the lung, liver, and intestine. Ritonavir is one of the strongest CYP3A4 inhibitors, the onset of interactions is fast (< 48 hrs) and persists for several days after completing the course.
- First, inhaled antimuscarinincs are primarily renally eliminated and undergo minor or no metabolism through CYP450 enzymes; so ‘no worries’ on these interacting
- Second, essentially all inhaled and systemic corticosteroids undergo significant metabolism by CYP3A4 and interact with Paxlovid®.
A study of ritonavir and prednisone in normals showed ~40% increase in blood levels with 4 days of ritonavir; 14 days of ritonavir led to levels persistently elevated. It is well-documented that systemic exposure of ICS increases with CYP3A4 inhibitors (eg – itraconazole) or decreases with inducers (eg – rifampin). Ritonavir has been reported to cause Cushings Syndrome in HIV patients receiving inhaled fluticasone propionate.
Likely, it is appropriate to continue ICS monotherapy while on Paxlovid®. The ICS dose and potency, and underlying comorbidities will affect the risk of ADRs. There’s conflicting evidence on the clinical benefits of ICS in COVID infections. - Third, interactions between some LABAs and ritonavir could be significant through adverse CV and metabolic effects. Use of albuterol or initiating prednisone may increase LABA risks. Much has been published about LABAs and CV risks in susceptible patients.
Salmeterol products (SEREVENT®, ADVAIR®, Wixela®, Airduo®) are essentially contraindicated with Paxlovid® because of 16-fold increases in blood levels when given with ketoconazole. Ketoconazole is a prototype for CYP3A4 inhibitor and intestinal P-gp transporters per FDA. It is assumed because salmeterol is dependent on CYP3A4 metabolism for systemic clearance, an interaction will occur with the strong inhibitor ritonavir.
Vilanterol (ANORO®, BREO®, TRELEGY®) metabolism is principally dependent on CYP3A4 and P-glycoprotein transporters. In a study reported in the PI, nearly a 2-fold increase in blood levels can occur with concurrent ketoconazole. Importantly, the vilanterol PI’s state to not use with strong CYP3A4 inhibitors, citing ritonavir; while some resources report no modification is needed.
Eight to ten days or longer of greater systemic exposure of salmeterol or vilanterol is a concern in patients receiving Paxlovid®, particularly the elderly with multi-morbidities present. A salmeterol PI warning was added many years ago for increased risk of death with overuse.
Olodaterol (Stioloto®, Striverdi®), arformoterol (Brovana®), and formoterol (multiple MDI, Perfomomist®) are unlikely to interact due to reliance on other CYP450 isozymes. - Fourth, these same issues are even more relevant when itraconazole, posaconazole, and possibly voriconazole due to strong CYP3A4 inhibition and frequent long courses.
- Marazolini et al. Recommendations for the management of drug-drug interactions between the COVID-19 antiviral nirmatrelvir/ritonavir (Paxlovid) and comedications. Clin Pharmacol Ther. 2022. Doi:10.1002/cpt.2646
- (https://www.covid19-druginteractions.org/checker)
WANT TO JOIN THE NORTH CAROLINA THORACIC SOCIETY?
https://www.thoracic.org/members/chapters/thoracic-society-chapters/north-carolina/
Officers – North Carolina Thoracic Society
President: Mashael Al-Hegelan, MD; Durham, Assistant Professor, Duke University Division
of Pulmonary, Allergy, and Critical Care Medicine
Vice President: Praveen Mannam, MD, Greensboro, Cone Health
Secretary-Treasurer: Sweta Patel, MD; Durham, Assistant Professor, Duke University
Division of Pulmonary, Allergy, and Critical Care Medicine
Chapter Councilor: Steve Tilley, MD; Chapel Hill, Associate Professor, UNC at Chapel Hill
Division of Pulmonary Diseases and Critical Care Medicine
Executive Director – Roy Pleasants, PharmD ncthoracicsociety@gmail.com
Newsletter Editor: Roy Pleasants, PharmD