“Advancing Lung Health in North Carolina”
North Carolina Thoracic Society Newsletter
Spring 2022
NCTS Events and Announcements
Newsletter Modification
Effective 2022, we will increase our number of newsletters to Spring, Summer, and Fall.
2022 NCTS Annual Educational Conference
Halleluiah, we had an in-person and virtual educational conference in Asheville March 26 with about 75 attendees, mostly from central and western NC. It was well-received and many felt it had an impact on their practice and personal life skills – thanks to our host James Davidson, MD who crafted this program (Asheville Pulmonary and Immediate Past-President).
https://duke.zoom.us/rec/share/h4I25scGKLMfc2ogWaO10MjBM8WJD7XzjyTw0zKII83dPFD ESZ070MNFEKFiOmWH.mW0cXA1gDIc3f3mc?startTime=1648294626000
Among the lectures, President-Elect of ATS – M. Patricia Rivera, MD – presented the new guidelines on lung cancer screening. Dr Rivera just left UNC after many years to become the new Chief at the University of Rochester. Craig Rackley, MD presented ECMO from H1N1 to Covid-19, followed by a discussion with the Cardiothoracic Surgeon who directs the ECMO program at Mission St Joseph (Jesse Madden, MD). Certainly impactful to practitioners based on feedback, but also highlights different practice models used for ECMO across our state.
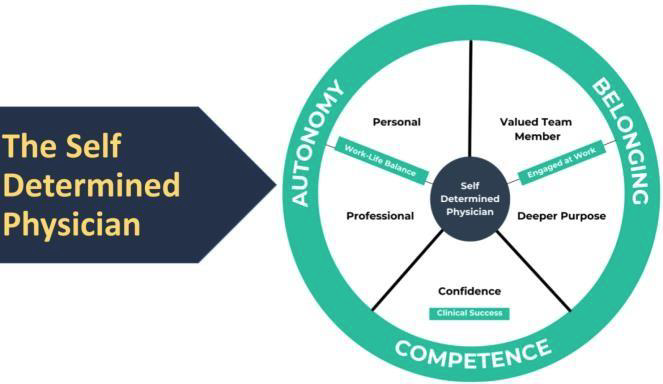
Jimmy Turner, MD (Anesthesiologist at Atrium-WFU and CEO The Physician Philosopher) provided insights into the professional and personal factors contributing to job satisfaction and burnout. He had some great messages.
Along the lines of life skills was the NCTS Clinician of The Year Award to Joe Govert, MD (Duke Pulmonary). Many who have worked with Joe agree he may be one of the best pulmonary clinicians in the country. Neil MacIntyre, MD(Duke Univ) presented the award, and both he and Joe acknowledged the tremendous contributions Joe’s family made.
Chad Marion, DO, PhD (WFU) presented on non-CF bronchiectasis and among the great info he presented, he highlighted there are no US guidelines on this condition. Aaron Vose, MD and Matt Makowski, MD (Duke), Benjamin Sines, MD (UNC), and Matthew Schertz, MD(WFU) presented their research. And of course, faculty from their respective programs asked tough questions!
Upcoming NCTS Meeting
NCTS will host a meeting entitled “Digital Health in Respiratory Diseases” on Saturday Sept 24 on the Duke University campus, under the direction of Mashael Al-Hegelan, MD, Praveen Mannam, MD, and Roy Pleasants, PharmD. Topics on the agenda include telehealth visits, remote digital monitoring for OSA, digital inhalers, remote pulmonary rehabilitation, “wearables” for lung diseases. Details to follow.
DISEASE UPDATE
Pulmonary Hypertension in COPD
Talal Dahhan, MD, MSEd
Assistant Professor, Duke University Division of Pulmonary, Allergy & Critical Care Medicine Specialist in Pulmonary Hypertension & Critical Care Medicine
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitations that is progressive. It is associated with abnormal inflammatory response to different stimulants in the air. COPD affects more than 13 million adults in the United States on annual basis. COPD deaths are significantly related to complications of this progressive disease.1 Pulmonary Hypertension (PH) is one of them, and it leads to right ventricular failure that is called “cor pulmonale”.2 3
COPD progression leads to hypoxemia. This may result in endothelial dysfunction. Maladaptive response of the pulmonary artery endothelium leads to hypoxic vasoconstrictive response due to several mechanisms. Unrecognized hypoxemia in COPD patients leads to development of these maladaptive responses and that results in significant rise in pulmonary vascular resistance (PVR). Pulmonary hypertension develops then and adds pressure on the right ventricle. Overtime, right ventricular (RV) failure and hypertrophy develop leading to more dyspnea, syncope, and death.2
Early recognition of hypoxemia and maintaining adequate oxygenation should result in reduction of these responses. Regular assessment of oxygenation with activity should arrest PVR rise. Performing oxygen titration assessments should be performed regularly for these patients to avoid development of cor pulmonale. Diuresis is important when RV failure is clinically overt.3
Recent advances in therapeutics for pulmonary hypertension in the setting of underlying interstitial lung disease has shined light for patients with advanced COPD and cor pulmonale who failed to have a response with conventional therapies. The INCREASE trial has included several patients with combined pulmonary fibrosis and emphysema (CPFE) syndrome. Patients who received inhaled Treprostinil (iTRE), had improvement in their functional capacity, assessed by six-minute walk distance.4 The PERFECT trial is currently randomizing patients with COPD who have developed PH, to receive iTRE versus placebo. Hopefully, we have results of this trial soon.5
References
1. Brown, D. W., Pleasants, R., Ohar, J. A., Kraft, M., Donohue, J. F., Mannino, D. M., Liao, W., & Herrick, H. (2010). Health-related quality of life and chronic obstructive pulmonary disease in North Carolina. North American journal of medical sciences, 2(2), 60–65. https://doi.org/10.4297/najms.2010.260
2. Shujaat, A., Minkin, R., & Eden, E. (2007). Pulmonary hypertension and chronic cor pulmonale in COPD. International journal of chronic obstructive pulmonary disease, 2(3), 273–282.
3. Weitzenblum, E., & Chaouat, A. (2009). Cor pulmonale. Chronic respiratory disease, 6(3), 177–185.
4. Waxman, A., Restrepo-Jaramillo, R., Thenappan, T., Ravichandran, A., Engel, P., Bajwa, A., Allen, R., Feldman, J., Argula, R., Smith, P., Rollins, K., Deng, C., Peterson, L., Bell, H., Tapson, V., & Nathan, S. D. (2021). Inhaled Treprostinil in Pulmonary Hypertension Due to Interstitial Lung Disease. The New England journal of medicine, 384(4), 325–334.
5. http://clinicaltrials.gov NCT03496623
Environment and Lung Health
Health Equity, Air Quality, and Climate Change
Andrew Harver, PhD Professor of Public Health Sciences, UNC Charlotte
As we are too aware SARS-Cov-2 has not only exhausted front-line health care providers – fragmenting the routines we are only learning to put back in place back in place – but also exacerbated long-standing social and health inequities, including those related to poor air quality fueled by climate change. More than 4 in 10 Americans breathe unhealthy air, and people of color are three times as likely to live in the most polluted places. Blacks and
American Indian/Alaska Natives have the highest current asthma rates
compared to other races and ethnicities; and the health impacts of climate change are inequitable, with disproportionate effects on the most susceptible populations in every society, 4
including people with low incomes, members of minority groups, women, children, older adults, people with chronic diseases and disabilities, and outdoor workers. These facts reveal a deeper question of justice, whereby climate change may interact with existing social and economic inequalities to exacerbate enduring trends not only within countries but also between neighborhoods to include historic levels of air pollution and proximity to energy and industrial facilities. The NC Clinicians for Climate Action, representing “public health practitioners, physicians, nurses, and allied health professionals across North Carolina” recognize climate change as a public health emergency. In this regard, the Lancet Countdown on health and climate change reminds us that “Climate change is the greatest global health threat facing the world in the 21st century, but it is also the greatest opportunity to redefine the social and environmental determinants of health.”
Journal Club – Inhaled Steroids
Prepared by Roy Pleasants, PharmD (Executive Director, NCTS)
“Metabolomic profiling reveals extensive adrenal suppression due to inhaled corticosteroid therapy in asthma.” Kachroo et al Nature Medicine 2022(PDF only for purposes of reading this discussion)
Study goals: Determine the hormonal suppressive effects of ICS based on the asthmaspecific plasma profiles of steroid hormone metabolites among pediatric asthmatics, adult asthmatics, and controls – with and without ICS use, and accounting for OCS use Study Population: Asthmatics and non-asthmatics(control) from 4 cohorts
1) European Prospective Investigation of Cancer-Norfolk (EPIC): 661 adult asthma,
10754 controls
a. Discovery cohort to determine metabolomic profile of steroid hormone metabolites in asthma and controls, irrespective of ICS exposure
2) Mass General Brigham Biobank-Asthma (MGBB): 287 adult asthma, 323 controls
a. Replication cohort to determine metabolomic profile of hormone metabolites associated with prevalent asthma, and to assess contribution of ICS
3) Childhood Asthma Management Program (CAMP): 560 pediatric asthmatics (RCT,
Budesonide vs Nedocromil vs Placebo)
a. Long-term cohort for ICS use and adrenal suppression
4) Electronic Medical Record: Cortisol (EMR-C): 383 asthma, 1852 controls
a. Validation cohort for 24 hr adrenal suppression among patient pop, employing ACTH stim (MGB EMR)
Procedures:
1) Measurement of plasma metabolites (LC, mass spec) from steroid hormone pathways to determine the metabolomic profile most associated with prevalent asthma; employing large epidemiologic studies (EPIC, MGBB)
- 2) Using the selected metabolomic profile: (MGBB) a. Compared asthma vs non-asthma
- b. Compared asthma ICS users vs asthma non-ICS users
5
- c. Determined dose-dependency
i. Low-dose fluticasone propionate (44-200 mcg/d) vs high-dose (>200 mcg/d)
3) Assessed long term (4 yrs) adrenocorticoid suppression in children using low-dose ICS (CAMP)
4) Compared cortisol levels in patients with ACTH stim tests among a patient population(EMR-C) a. No asthma/no ICS
b. No asthma/ICS
c. Asthma/no ICS
d. Asthma/ICS
Findings:
1) Beginning with > 900 metabolites of pregnenolone, androgens, glucocorticoids, and progestins, researchers identified a metabolomic profile of 17 significantly associated with prevalent asthma (EPIC, MGBB)
a. These 17 metabolites were reduced among adult asthmatics regardless of ICS use
2) Largest reductions in metabolites occurred with ICS treatment (MGBB)
3) Effects on steroid metabolites were dose dependent(MGBB); however, reductions also occurred with low-dose ICS treatment in adults and children (MGBB,CAMP)
4) Increased risk of adrenal insufficiency and non-specific clinical findings (anemia and fatigue) with ICS use (EMR-C)
Weaknesses:
1) Did not account for all confounders among cohorts
2) Only applied complete metabolomic profiling to epidemiology studies
3) Partial assessment of systemic adverse effects of ICS; No comparisons among ICS
Significance:
1) In the most comprehensive study of hormonal suppressive effects of ICS in asthma, researchers identified a profile of reduced steroid hormone metabolites associated with prevalent asthma, that were further lowered by ICS
2) While most focus on cortisol suppression, other steroid hormones are also reduced by ICS
a. Eg bone effects of CS in part due to effects on androgens
3) Suppression of cortisol was dependent on the ICS dose, but was evident at low doses and was sustained over time
Comments:
Systemic adverse-effects of ICS are not fully known, especially over a lifetime; but we do know for all routes of corticosteroids, side-effects are dose-, potency-, and durationdependent. It took more than 10 years to recognize the pneumonia risk with potent ICS. Considered preliminary, but of concern are reports suggesting higher risk of diabetes, cataracts, and osteoporosis with long-term ICS. Recognizing ICS are a core 6
part of asthma management and some patients need high doses, strategies to lower cumulative exposure to ICS need to be considered.
Kachroo_et_al-2022-
Nature_Medicine.pdf
WANT TO JOIN THE NORTH CAROLINA THORACIC SOCIETY?
Officers – North Carolina Thoracic Society
President: Mashael Al-Hegelan, MD; Durham, Assistant Professor, Duke University Division of
Pulmonary, Allergy, and Critical Care Medicine
Vice President: Praveen Mannam, MD, Greensboro, Cone Health
Secretary-Treasurer: Sweta Patel, MD; Durham, Assistant Professor, Duke University
Division of Pulmonary, Allergy, and Critical Care Medicine
Chapter Councilor: Steve Tilley, MD; Chapel Hill, Associate Professor, UNC at Chapel Hill Division of Pulmonary Diseases and Critical Care Medicine
Executive Director – Roy Pleasants, PharmD ncthoracicsociety@gmail.com