Message from the President
Mashael Al-Hegelan, MBBS (Duke University Division of Pulmonary, Allergy and Critical Care Medicine
Greetings!! I hope this newsletter finds you all healthy and well. Over the last few years, it has been a pleasure to be a member of NC Thoracic Society and a privilege to serve on the executive leadership team for the last 2 years.
During the COVID-19 pandemic, our PCC society as a whole rose to the challenge in caring for our patients with this disease. Almost two years now into the pandemic, we are all experiencing burnout. It is a real thing. We are all tired, exhausted, and disheartened by much of what happening around the country and the world today. As a chapter within ATS, I am proud of how our national and local society stepped up. I am appreciative and in awe of everyone’s contributions to creating tools, guidance documents, published research, patient resources, webinars, podcasts, and resources about vaccines, and how we all pivoted our work to virtual platforms, continued to innovate and leverage lessons learned. All the while continuing to provide unwavering dedication to the clinical care of our patients. Despite everything, you all showed up and gave it 100% all the time, and for that you have my respect and heartfelt gratitude. I know first-hand how important a community like NCTS is.
As a foreign medical graduate who moved to the US in 2006, it was not easy navigating the US medical system. I initially joined the Duke IM residency followed by the PCC fellowship before becoming a faculty member. For many years I found it challenging to connect with local PCC specialists from both academic and private practices. Formed in 2017, a state chapter of ATS, the NCTS which provided an annual educational conference, was a great opportunity for me to get to know and connect with my colleagues and fellow Pulmonary & Critical Care specialists across the state.
Just like I found solace in connecting with my peers through ATS and NCTS, then and now, I am
confident you will too. I sincerely hope we will all continue to reach out and connect through
this society to share our stories, our concerns, and ideas, and to continue to feel supported
during this challenging time in medical history.
Over the coming year, we have several NCTS events planned. Unfortunately, our annual
educational conference previously scheduled for September in Asheville, had to be postponed
given the rise in COVID-19 cases in the state at the time. Our dedication to you and your safety
is paramount and our main priority, so in lieu of a virtual conference, we decided to postpone it
until it we were able to meet in person. Our new meeting date is now scheduled for March 26 th
in Asheville.
At NCTS we strive to continue to engage and connect all providers from academic and private
practices across the state, and I sincerely hope you find these connections as enriching as I do.
Over the coming year, we plan to continue to offer virtual and in-person educational meetings
and conferences, and sincerely hope you are able to join us.
Finally, I would like you to help me extend a warm welcome to our new executive leadership
members; Sweta Patel, MD who will be joining as Secretary/Treasurer and Stephen Tilley, MD 2
who will be serving as our chapter counsellor.
All of us at NCTS would sincerely appreciate you consider joining our society. Please visit our
website for more information and educational material www.NCTHORACIC.org To join, follow the link: https://www.thoracic.org/members/chapters/thoracic-society-chapters/north-carolina/
Sincerely,
Mashael Alhegelan, MD
North Carolina Thoracic Society President
NCTS Events and Announcements
Postponement of 2021 NCTS Annual Education Conference
Our annual educational conference is re-scheduled Saturday March 26, 2022 at the Asheville Doubletree Biltmore. We are still finalizing the agenda, but expect it to be quite similar to the original program. It is a great place to bring friends and family, and we will all be eager to enjoy the early Spring.
Additional Meetings and Conferences
NCTS will facilitate two or more Meet The Professor hybrid meetings in 2022. Let us know if there is a topic you would like to offer for your practice. These sessions are part of NCTS’s outreach to engage pulmonary specialists throughout the state.
As we are having our ‘annual’ 2021 educational conference in 2022, we will not have a second annual conference in 2022. Instead we will have a focused meeting late summer on digital telehealth at Duke University.
New Officers

Sweta Patel, MD, MS (Duke University) is the new Secretary-Treasurer for NCTS 2021-2022. Sweta is a North Carolina native and completed her undergraduate and medical degrees at Duke University. After completing an internal medicine residency at the University of California, San Francisco, she returned to Duke for her combined fellowship in Pulmonary and Critical Care Medicine and Global Health. She is now an Assistant Professor of Medicine and Global Health at Duke University. Her research focuses on the respiratory microbiome in people with HIV and COPD in Botswana.

Steve Tilley, MD (UNC Chapel Hill) is the new Chapter Councilor for NCTS for 2021- 2023. The Councilor serves as a liaison between NCTS and ATS. Steve is Associate Professor at UNC CH Division of Pulmonary Diseases and Critical Care Medicine. He has spent his career doing basic and clinical research, and is active teaching in the Division and medical school. He is Director of the UNC Adult Asthma Program and practices in a outpatient clinic and in the medical ICU. 3
North Carolina Thoracic Society’s 2021 Outstanding Clinician Awardee
Joseph A. Govert, MD (Duke University) is being awarded the North Carolina Thoracic Society’s 2021 Outstanding Clinician of the Year. As part of this award, the Society is nominating Joe to the ATS Respiratory Health Awards as the 2022 ATS National Clinician of the Year. He will receive the NCTS award at the next Annual Educational Conference Spring 2022. He has been a committed clinician and educator with Duke Pulmonary, Allergy, and Critical Care Division since 1988, serving in many roles. His extensive clinical experience and knowledge of so many aspects of hospital and outpatient pulmonary care are remarkable. His bedside manner is worthy of the best. He has received nine teaching awards and his patients routinely report he is one of the best physicians they have had. Notably, Joe has achieved full Professor at Duke University School of Medicine, largely based on these skills.
FELLOWS CORNER
Oscillometric Testing: Overview and Clinical Implications for Adult Patients
Aaron Vose, MD (Duke University)
Spirometric pulmonary function testing remains the gold standard for diagnosis and characterization of airways disease, but limitations remain. One significant drawback is the reliance on patient effort to provide accurate data, particularly when assessing the small airways. Oscillometry represents an opportunity to overcome this limitation, as well as allowing airways testing to be performed among adult patients who could not otherwise perform spirometry (e.g. weakness, recent surgery, or pneumothorax).
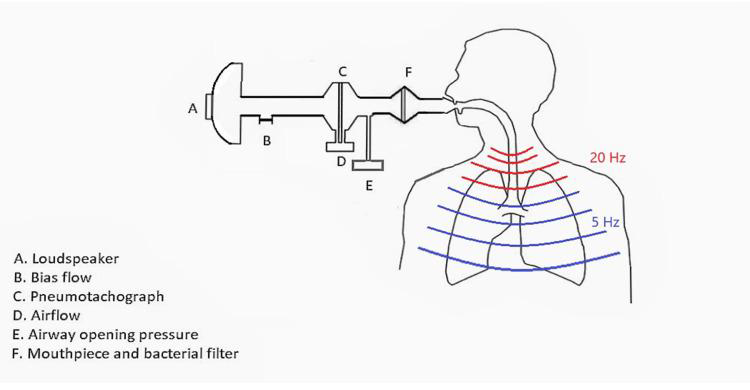
Oscillometry is a passive maneuver in which a patient practices seated, tidal breathing while a sound generator applies sound waves from 5 to 30Hz into the respiratory tract. [1] High frequencies measure large airways, while low frequencies reach distal airways and parenchyma. These waves then return to the oscillometer and provide quantitative measures of airways resistance in both large and small airways, as well as data suggesting degree of pulmonary compliance. [2]
Oscillometry has been well validated in pediatric patients, particularly in diagnosis of asthma and measure of airways disease reversibility. In adults, oscillometry has been utilized to diagnose airways disease and their exacerbations, assess bronchodilator responsiveness in
asthma and COPD, and create correlates with dyspnea scores. [3-6] Unfortunately, due to lack
of generalizable references equations and overall practitioner familiarity with spirometry,
oscillometry is not yet widely utilized in the adult population. I am currently using consecutively collected spirometry and oscillometric measures to isolate chest wall effects and look for unique signatures of small airways disease in obese individuals at the Durham VA.
Oscillometry represents an opportunity to be more specific in our ability to measure airways
disease and response to therapy, particularly among patients with airways disease or otherwise unable to perform traditional spirometry. 4
Figure 1: Overview of Impulse Oscillometry Design and Sound flow [3]
1. Dubois, A.B., et al., Oscillation mechanics of lungs and chest in man. J Appl Physiol, 1956. 8(6): p. 587-94.
2. Contoli, M., et al., The small airways and distal lung compartment in asthma and COPD:a time for reappraisal. Allergy, 2010. 65(2): p. 141-51.
3. Porojan-Suppini N, Fira-Mladinescu O, Marc M, Tudorache E, Oancea C. Lung Function Assessment by Impulse Oscillometry in Adults. Ther Clin Risk Manag. 2020 Nov 26;16:1139- 1150. doi: 10.2147/TCRM.S275920. Erratum in: Ther Clin Risk Manag. 2021 Feb 02;17:135.
PMID: 33273817; PMCID: PMC7705955.
4. Borrill, Z.L., et al., Measuring bronchodilation in COPD clinical trials. Br J Clin Pharmacol, 2005. 59(4): p. 379-84.
5. Nielsen, K.G. and H. Bisgaard, Discriminative capacity of bronchodilator response measured with three different lung function techniques in asthmatic and healthy children aged 2 to 5 years. Am J Respir Crit Care Med, 2001. 164(4): p. 554-9.
6. Ren, C.L., et al., Changes in lung function measured by spirometry and the forced oscillation technique in cystic fibrosis patients undergoing treatment for respiratory tract exacerbation. Pediatr Pulmonol, 2006. 41(4): p. 345-9.
DISEASE UPDATE

The Changing World of Cystic Fibrosis: An Update on Highly Effective Modulator Therapy
Jennifer Goralski, MD; Associate Director, Adult Cystic Fibrosis Clinic; The University of North Carolina at Chapel Hill
2020 marked a year that few will soon forget due to the coronavirus pandemic, but for people living with cystic fibrosis (CF), 2020 may have also been the first year in their lives where they were not hospitalized to treat a CF pulmonary exacerbation. In October 2019, the FDA approved elexacaftor/tezacaftor/ivacaftor (E/T/I) for people with CF aged 12 and older who are homozygous for the F508del mutation or heterozygous for F508del and a minimal function mutation. This small molecule compound corrects and enhances the function of the cystic fibrosis transmembrane conductance regulator (CFTR) protein, the underlying genetic defect in CF. Pivotal studies showed substantial clinical efficacy in patients who were treated with the oral combination therapy, with marked improvements in FEV1, BMI, and daily symptoms, as well as a decline in sweat chloride values (1, 2). Moreover, additive benefit was seen when patients with a gating or residual function mutation were transitioned from ivacaftor to E/T/I therapy (3). In December 2020, the FDA expanded the indication to include an additional 177 rare mutations based on the results of in vitro theratyping, a process for personalized medicine where mutations are matched with therapies in a lab setting, a crucial step in gaining access to treatments for extremely rare disorders. An open-label extension study demonstrated ongoing clinical benefit (4) and FDA approval was extended down to age 6 in June 2021 based on phase 3 trials showing safety and efficacy in this age group (5). Studies in children ages 2-5 are ongoing (NCT04537793).
Thus, there has been a paradigm shift in CF care. While research into the optimal care of pulmonary exacerbations and advanced lung disease remains critical (6, 7), researchers are increasingly delving into topics of high priority to patients, including studying the broader impacts of highly effective modulator therapy (8), fertility and family planning (9), and the potential tradeoffs of 5
stopping chronic (and time-consuming) aerosolized therapies (10) in stable CF lung disease. Simultaneously, work continues in genetic therapies proposed for patients who are ineligible for, or intolerant of, CFTR modulators. With these advances and others, the landscape of CF clinical care and research is rapidly evolving.
1. Heijerman HGM, McKone EF, Downey DG, Van Braeckel E, Rowe SM, Tullis E, et al. Efficacy and safety of the elexacaftor plus tezacaftor plus ivacaftor combination regimen in people with cystic fibrosis homozygous for the F508del mutation: a double-blind, randomised, phase 3 trial. Lancet. 2019;394(10212):1940-8.
2. Middleton PG, Mall MA, Drevinek P, Lands LC, McKone EF, Polineni D, et al. Elexacaftor-Tezacaftor-Ivacaftor for Cystic Fibrosis with a Single Phe508del Allele. N Engl J Med. 2019;381(19):1809-19.
3. Barry PJ, Mall MA, Alvarez A, Colombo C, de Winter-de Groot KM, Fajac I, et al. Triple Therapy for Cystic Fibrosis Phe508del-Gating and -Residual Function Genotypes. N Engl J Med. 2021;385(9):815-25.
4. Griese M, Costa S, Linnemann RW, Mall MA, McKone EF, Polineni D, et al. Safety and Efficacy of Elexacaftor/Tezacaftor/Ivacaftor for 24 Weeks or Longer in People with Cystic Fibrosis and One or More F508del Alleles: Interim Results of an Open-Label Phase 3 Clinical Trial. Am J Respir Crit Care Med. 2021;203(3):381-5.
5. Zemanick ET, Taylor-Cousar JL, Davies J, Gibson RL, Mall MA, McKone EF, et al. A Phase 3 Open-Label Study of Elexacaftor/Tezacaftor/Ivacaftor in Children 6 through 11 Years of Age with Cystic Fibrosis and at Least One F508del Allele. Am J Respir Crit Care Med. 2021;203(12):1522-32.
6. Southern KW, Murphy J, Sinha IP, Nevitt SJ. Corrector therapies (with or without potentiators) for people with cystic fibrosis with class II CFTR gene variants (most commonly F508del). Cochrane Database Syst Rev. 2020;12(12):Cd010966.
7. Djavid AR, Thompson AE, Irace AL, Gusman E, Altman K, DiMango EA, et al. Efficacy of Elexacaftor/Tezacaftor/Ivacaftor in Advanced Cystic Fibrosis Lung Disease. Ann Am Thorac Soc. 2021.
8. Nichols DP, Donaldson SH, Frederick CA, Freedman SD, Gelfond D, Hoffman LR, et al. PROMISE: Working with the CF community to understand emerging clinical and research needs for those treated with highly effective CFTR modulator therapy. J Cyst Fibros. 2021;20(2):205-12.
9. Taylor-Cousar JL, Jain R. Maternal and fetal outcomes following elexacaftor-tezacaftor-ivacaftor use during pregnancy and lactation. J Cyst Fibros. 2021;20(3):402-6.
10. Mayer-Hamblett N, Nichols DP, Odem-Davis K, Riekert KA, Sawicki GS, Donaldson SH, et al. Evaluating the Impact of Stopping Chronic Therapies after Modulator Drug Therapy in Cystic Fibrosis: The SIMPLIFY Clinical Trial Study Design. Ann Am Thorac Soc. 2021;18(8):1397-405.

PATIENT PERSPECTIVE
Camryn Kellogg (UNC Chapel Hill Student) How my local environment impacted my asthma
Hello everyone- my name is Camryn Kellogg, and I am currently a senior Morehead-Cain Scholar at UNC! I’d like to take this opportunity to share my family’s story in our fight against asthma.
My entire family is from Western Massachusetts where I was born and raised. From an early age, I began to struggle with my breathing. I vividly remember the terrifying experience of my first asthma attack, and the many late-night trips to the ER as my asthma progressively worsened. By the time I was in second grade, my sister and I were told we would need to take prednisone daily to control our asthma. My newborn brother was headed down the same road, and that is when our pediatric pulmonologist, Dr. Paul Salva, recommended we move to a warm, coastal climate to improve our quality of life.
Dr. Salva hypothesized that the higher temperatures and humid environment would benefit us considering our lungs were sensitized to the harsh, dry cold of the north. Further, he believed the constant breeze of the ocean would act as an air filter, preventing pollutants from settling like they did in Western Massachusetts. After making the move in elementary school, my entire quality of life improved dramatically. I went from missing weeks of school to playing the saxophone, from sitting on the sidelines at soccer to starring in my school’s musical. By the time I was in high school, I started an asthma support-group & awareness club at my school, and founded an annual asthma walk in Wilmington to benefit the American Lung Association.
In 2016, the ALA connected my family and I with the Environmental Protection Agency. We gave an interview to the EPA describing our move and support of the Clean Power Plan, and shortly after received an invitation to the White House. President Obama had heard about our relocation and advocacy work, and wanted to personally thank us. After our meeting, he invited me to stand behind him as he unveiled the plan to the country, an experience I will never forget. I have since continued my advocacy work at UNC, where I’ve founded the AIR Club to raise awareness about lung health and have conducted asthma-related research in the Tilley Lab.
I am very grateful for the opportunity to share my story, and I am extremely grateful that my asthma today is well-controlled and no longer dominates my life. If anyone would like to reach out and discuss their experience with asthma or learn more specifics about the AIR Club or my research, feel free to email me at ckellogg@live.unc.edu.
Editor’s note: We are hoping to convince Camryn to pursue a career in pulmonary medicine!! 6
Officers – North Carolina Thoracic Society
President: Mashael Al-Hegelan, MD; Durham, Assistant Professor, Duke University Division of Pulmonary, Allergy, and Critical Care Medicine
Vice President: Praveen Mannam, MD, Greensboro, Cone Health
Secretary-Treasurer: Sweta Patel, MD; Durham, Assistant Professor, Duke University Division of Pulmonary, Allergy, and Critical Care Medicine
Chapter Councilor: Steve Tilley, MD; Chapel Hill, Associate Professor, UNC at Chapel Hill
Division of Pulmonary Diseases and Critical Care Medicine
Executive Director – Roy Pleasants, PharmD ncthoracicsociety@gmail.com